Posted
14th February 2022
Research
This week’s article is a summary of the latest guidelines published for the management of MRSA. It includes a study where the introduction of Clinell Universal Wipes resulted in a 55% reduction in the rate of MRSA acquisition. Read on to find out more.
New guidelines have been published regarding the management of methicillin-resistant Staphylococcus aureus (MRSA). The guidelines were jointly produced by the Healthcare Infection Society and Infection Prevention Society, both of which are leading societies for advising on infection prevention and control (IPC) practice and guidelines.
The guidelines cover a range of areas and role of areas such as:
- Skin decolonisation and use of skin antiseptics
- Cleaning and disinfection
- Screening
- Education and use of feedback
What is MRSA?

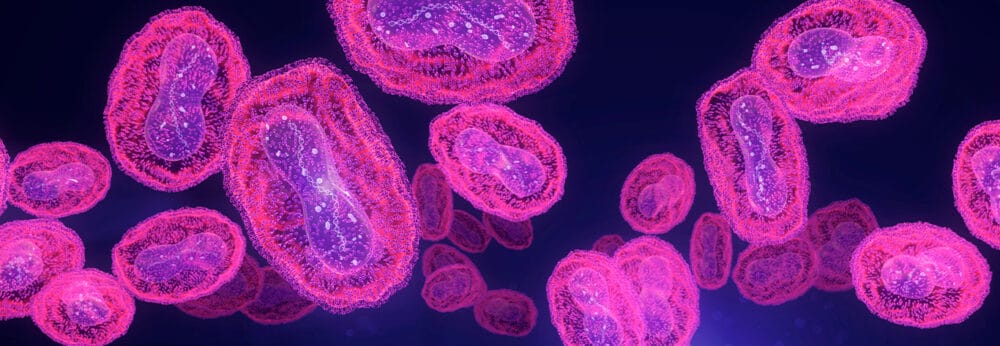
MRSA is a Gram-positive bacterium which can cause of range of infections. MRSA infections are frequently observed in people with underlying health conditions and can occur when care is given (which can be in hospitals or in community settings such as residential homes). MRSA infections are often difficult to treat as it is resistant to some types of commonly used antibiotics, such as the penicillin family of antibiotics.
What are the guidelines for management of MRSA?
The last set of guidelines relating to management of MRSA were published in 2006. Since 2006 there have been numerous new publications, hence a requirement to update guidelines based on new evidence available. A systematic review (this is a review of literature on a certain subject area between a certain timeframe) was carried out and after reviewing the available evidence, the authors published a set of guidelines covering elements of MRSA management. The guidelines provide clinically effective measures for preventing transmission of MRSA. Some of the guidance is discussed in more detail below.
Decolonisation therapy in reducing MRSA acquisition and transmission
Decolonisation is the process of eradicating or reducing carriage of microorganisms on our skin which can be a benefit to reduce the risk of infection or transmission to others. Chlorhexidine (CHG) is a skin antiseptic, commonly used to decolonise people who carry potentially dangerous microorganisms on their skin (including MRSA and Carbapenemase-producing Enterobacterales (CPE)). The authors found strong evidence for the benefits of CHG, with various studies demonstrating effectiveness of CHG on the prevalence of MRSA colonisation, and incidence of acquisition and infection.
Amongst the evidence reviewed was a published study where the use of GAMA 2% CHG bathing wipes significantly decreased the trend of MRSA acquisition rates in an intensive care unit.

Recommendations and good practice for MRSA decolonisation:
- Use chlorhexidine, either selectively or universally, for body decolonisation to reduce MRSA carriage.
- For skin decolonisation, if 4% chlorhexidine wash is used, moisten the skin, apply the wash, and leave for 1–3min before rinsing off; if 2% chlorhexidine wipes are used, do not rinse off.
Reducing contamination of the environmental and shared equipment to minimise transmission of MRSA
Environmental decontamination has a role to play in reducing the risk of transmission and there’s specific evidence relating to the impact on MRSA. The guidelines reviewed published studies which examined a range of methods for environmental decontamination including disinfectant agents (such as quaternary ammonium compounds and bleach), automated room disinfection (such as ultraviolet light) and antimicrobial surfaces.
Amongst the studies included was a study conducted at University Hospitals Birmingham where the introduction of our Clinell Universal Wipe resulted in a 55% reduction in the rate of MRSA acquisition.
Another study analysed, linked an MRSA outbreak to contaminated anaesthetic equipment which had been inappropriately disinfected. Introducing enhanced disinfection (use of ultraviolet light) resulted in the outbreak being controlled.
Following recommendations and good practice points were made:
- Clean and disinfect shared pieces of equipment used in the delivery of patient care after each use.
- Consider hydrogen peroxide vapour (HPV) or ultraviolet light as an adjunct to terminal cleaning as a part of a wider IPC strategy.
- Make all healthcare workers aware of the importance of maintaining a clean and safe care environment for patients ensuring staff are aware of specific responsibilities for cleaning and decontaminating the clinical environment.
Various other elements of MRSA management are discussed in the guidelines, including universal screening for staff and patients, surveillance and feedback for staff and the use of contact precautions.
Are the guidelines relevant outside of the UK?
As the recommendations are based on a systematic review of UK and international literature the recommendations are applicable to a wider international audience.
Summary
It is welcoming to see these guidelines being reviewed and updated to reflect developments and publications in the area of MRSA management. Generation of guidelines following the review of evidence in a systematic approach, allows healthcare professionals to focus their efforts in providing the highest standard of patient care possible.
If you’re interested in reading more research articles from GAMA, visit our Research page on our blog. Share this article on social media.
SHARE THIS ARTICLE
Tags
Latest News
Norovirus: Understanding its transmission and prevention in the UK
Introduction Norovirus is recognised as the leading cause of viral gastroenteritis…
Clean Between to Reduce Healthcare-Associated Infections
Healthcare-associated infections (HAIs) are a significant concern for healthcare facilities…
Mpox: emergence of a new threat
A new threat related to mpox is emerging, in the…
Wiping away infections – the CLEEN way!
Cleaning shared medical equipment with a disinfectant wipe at least…