Posted
29th July 2022
Research
Our Clinical Specialist for Capital, Claudia Santos, shares her personal experience of having COVID and what steps we should put in place to protect ourselves and those around us.
DISCLAIMER:
With a marked increase in the number of COVID cases over the last few months and having myself been infected with COVID on three separate occasions, I decided to write this blog post from the point of view of my own experience in the UK. I am grateful to be able to work in a company that allows me to express my opinions.
A year ago, on the 19th of July 2021, the British government announced the lifting of all COVID restrictions, on what later became known to many as “Freedom Day”.
However, a year on, and where exactly are we at? Do we have that so called ‘freedom’? The pandemic, along with all the other factors affecting our society (global warming, inflation, wars), have caused society to split and divide into groups. Those that have perhaps caught COVID, more than once, or worked in an environment that has demonstrated the effects that COVID infection can have, versus those individuals who have, in my opinion, been lucky enough to escape it for 2 years and are only now perhaps succumbing to the infection.
“The bottom line that ‘Covid is airborne’ has grown traction and deserved attention”
As a nurse by background, I first contracted COVID from one of my patients, at the very beginning of the pandemic in April 2020. At the time, there was still debate surrounding transmission and spread of SARS-CoV-2. Although there have been some studies that demonstrate that SARS-CoV-2 can, in some cases, survive on surfaces [1], the bottom line that “Covid is airborne” has grown traction and deserved attention.[2]
RELATED ARTICLE: Let’s keep ventilation open: Why The White House is clearing the air on COVID
I have since had another 2 reinfections, in July 2021 and March 2022, having received both my vaccinations and in addition the booster vaccine. I would not class myself as vulnerable or immunocompromised, and having left the NHS in September 2021, I can confidently say that the March infection was not related to my working environment, but rather everyday life that we all, as humans, have desperately wanted to get back to.
“2 million people in the UK are suffering from long COVID”
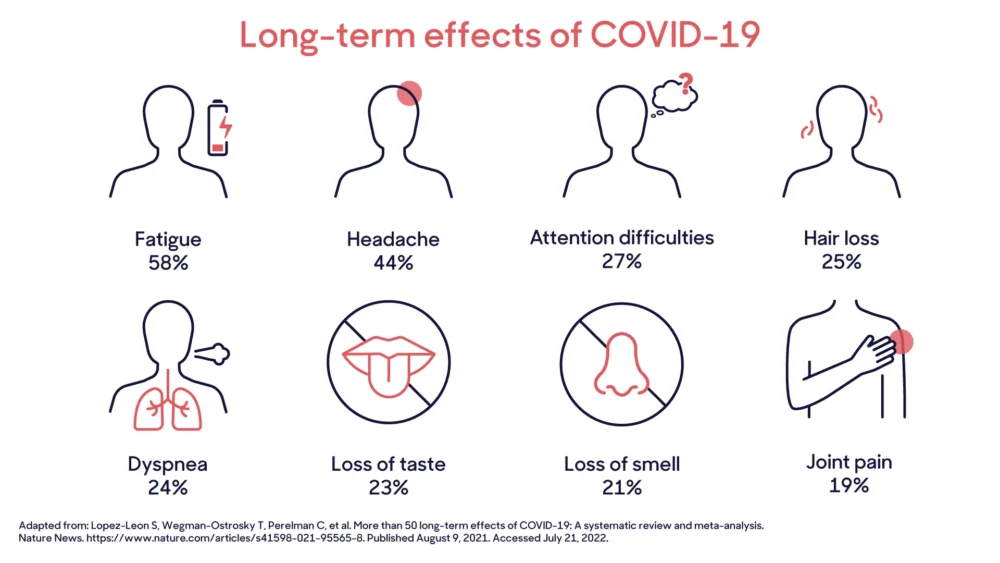
As a young, relatively fit woman with an interest in public health and a solid scientific background, my concern for the potential effects that these reinfections may have on me at a later stage in my life are mounting. Latest figures from the Office for National Statistics suggest that approximately 2 million people in the UK are suffering from long COVID,[3] with individuals experiencing a range of symptoms from fatigue and insomnia, to strokes and heart attacks. In fact, a recent systematic review published in Nature stated that there were over 50 long term effects of COVID infection, some of which are identified in the graphic below.[4]
RELATED ARTICLE: Covid Anxiety Syndrome and how to manage it
“The latest wave of COVID infections has resulted in an increase in hospitalisations”
The latest wave of COVID infections, driven by the variant BA 2.75, has resulted in an increase in hospitalisations and re-infections.[5] The WHO continues to monitor the BA 2.75 variant, which was first sequenced in India earlier in May. It has colloquially been named Centaurus, and although this nomenclature has not been approved by the WHO, this variant has an increased number of mutations that have enabled the virus to adapt toand evade the body’s immune response, thus increasing its transmissibility and ability to cause reinfections.[6]
Some may argue that the collapse in testing and reporting of infections means that the number of cases is likely a lot higher than figures quoted. To add to this figure, what about those individuals who are asymptomatic and might be unaware they are spreading infection or, perhaps those that are self-employed and, considering the increases in costs of living, have no choice but to work.
RELATED ARTICLE: Why taking care of the air makes our offices safer
“Now is the time to create environments that are infection resilient”
In the UK, the emphasis on COVID-19 guidance has shifted and focuses now on personal responsibility and this idea that we must ‘live with it’. However, for some individuals more susceptible to infection, this is not a viable solution. So how can we protect ourselves and our loved ones in the absence of clear public health messaging? One possible solution is to focus resources on creating infection resilient environments, whether that be in public spaces, schools, hospitals or even at home.
In the UK, school attendance has dropped by 70% since the beginning of the year and 1 in 5 children are absent from their schooling. According to statistics published by the Department for Education, attendance in the last month alone has dropped from 89.4% to 86.9%. [7] The impact of missed schooling on the education of children, our future leaders, has been well documented. With some school holidays fast approaching, perhaps now would be an ideal time to create environments that are, infection resilient, by installing or upgrading ventilation systems and in cases where this is not possible, mitigating it with the use of products such as Rediair.
“We have a social responsibility to those around us, to our children and the world we live in“

I think after the last two years of the pandemic, it’s clear that COVID and its many variants are here to stay. But to avoid this approach of just ‘living with it’ and potentially exposing ourselves to further problems down the line, maybe we should as individuals, look after ourselves and those around us, whether they be friends or neighbours. The 7 point plan [8] highlighted in the BMJ is a great starting point and a reminder to us all that we have a social responsibility to those around us, to our children and the world we live in.
[1] Dubey A, Kotnala G, Mandal TK, et al. Evidence of the presence of SARS‐COV‐2 virus in atmospheric air and surfaces of a dedicated Covid Hospital. Journal of Medical Virology. 2021;93(9):5339-5349. doi:10.1002/jmv.27029
[2] Duval D, Palmer JC, Tudge I, et al. Long distance airborne transmission of SARS-COV-2: Rapid systematic review. BMJ. 2022. doi:10.1136/bmj-2021-068743
[3] Daniel Ayoubkhani SK. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 7 July 2022. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK – Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases
/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/7july2022. Published July 6, 2022. Accessed July 21, 2022.
[4] Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Nature News. https://www.nature.com/articles/s41598-021-95565-8. Published August 9, 2021. Accessed July 21, 2022.
[5] Mary Van Beusekom | News Writer | CIDRAP News | Jul 06 2022. Newest omicron subvariants can evade boosters, antibody therapies. CIDRAP. https://www.cidrap.umn.edu/news-perspective/2022/07/newest-omicron-subvariants-can-evade-boosters-antibody-therapies. Published July 6, 2022. Accessed July 21, 2022.
[6] Wang Q, Guo Y, Iketani S, et al. Antibody evasion by SARS-COV-2 omicron subvariants BA.2.12.1, Ba.4, & ba.5. Nature News. https://www.nature.com/articles/s41586-022-05053-w. Published July 5, 2022. Accessed July 21, 2022.
[7] Attendance in education and early years settings during the coronavirus (COVID-19) pandemic, week 28 2022. GOV.UK. https://explore-education-statistics.service.gov.uk/find-statistics/attendance-in-education-and-early-years-settings-during-the-coronavirus-covid-19-outbreak. Published July 12, 2022. Accessed July 21, 2022.
[8] SAGE I. A seven point plan to suppress covid infections and reduce disruptions. BMJ. 2022. doi:10.1136/bmj.o1793
SHARE THIS ARTICLE
Tags
Latest News
Introducing HEXI HUB: A seamless transition in our product line
We’re pleased to announce an update to our product offering…
Innovative solutions for tackling Carbapenemase-producing Enterobacteriaceae (CPE) at King’s College Hospitals
King’s College Hospital NHS Foundation Trust, one of London’s largest…
Gloves Off: reducing unnecessary plastic waste during environmental cleaning and disinfection
In this blog, Dr Phil Norville discusses the momentum-gaining ‘Gloves…
Gloves Off: Navigating SDS sheets and skin safety claims in environmental decontamination products
In this blog, James Clarke (Head of R&D, Science &…