Posted
26th June 2018
Research
A study published in the Lancet Infectious Diseases provides further evidence that UV room decontamination reduces transmission in hospitals. The multicentre cluster-randomised study showed that introducing UV room decontamination for selected patient rooms resulted in a hospital-wide reduction in C. difficile and VRE acquisition compared with standard methods of decontamination.
This is a companion article to the BETR-D study that was published in the Lancet last year. This huge multicentre cluster-randomised study involved around 300,000 admissions to 9 hospitals over two years. The hospitals used a random sequence of terminal disinfection strategies for rooms of patients with selected target pathogens (C. difficile, MRSA, VRE, and Acinetobacter spp.). The disinfection strategies were:
- QAC disinfectant plus sodium hypochlorite for difficile (the reference method),
- QAC + UV plus sodium hypochlorite plus UV for difficile,
- Sodium hypochlorite + UV and
- Sodium hypochlorite.
The hospital-wide rate of acquisition of the target pathogens was investigated as a combined rate and for individual pathogens.
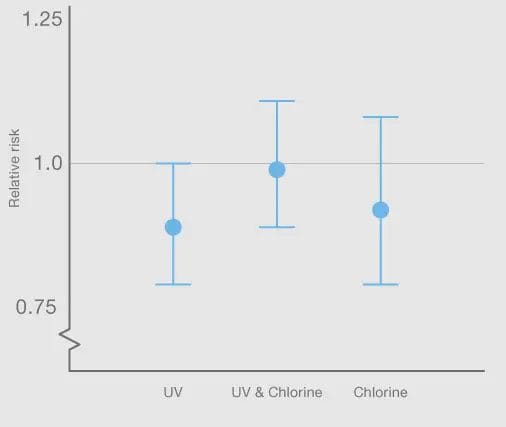
Overall, the QAC + UV proved to be the most effective strategy, with a relative risk of acquisition for all pathogens combined of 0.89 and with an upper confidence interval that just touched 1 (see Figure). This means that this reduction for all pathogens combined was right on the borderline of what would be considered statistically significant. This was driven by a statistically significant reduction in the acquisition of VRE (relative risk 0.56, confidence interval 0.31 – 0.996; p=0.048) and C. difficile (0.89, 95% CI 0.80 – 0.99; p=0.031).
Figure 1: The relative risk of acquiring all target pathogens combined for the test methods compared with the reference method, which was QAC disinfectant for all pathogens plus sodium hypochlorite for C. difficile
These findings are curious in some ways. The original BETR-D study showed that patients coming into rooms disinfected using UV were less likely to acquire target pathogens than patients admitted to rooms disinfected using standard methods. Here, the question was whether improved terminal disinfection would have a hospital wide impact, and this was shown to be the case for VRE and C. difficile. This suggests that improving terminal disinfection not only improves patient outcomes for the next patient to occupy a single room, but has knock-on clinical benefits measurable across the entire hospital!
These findings strengthen the case for enhancing terminal disinfection strategies by adding automated room decontamination systems, such as UV.
SHARE THIS ARTICLE
Tags
Latest News
Celebrating 20 Years of GAMA Healthcare: Our Story
This month, GAMA Healthcare celebrates 20 years of helping prevent…
Norovirus: Understanding its transmission and prevention in the UK
Introduction Norovirus is recognised as the leading cause of viral gastroenteritis…
Clean Between to Reduce Healthcare-Associated Infections
Healthcare-associated infections (HAIs) are a significant concern for healthcare facilities…
Mpox: emergence of a new threat
A new threat related to mpox is emerging, in the…