Posted
17th March 2022
Research
Our Clinical Specialist for Skin, Georgina Saviolaki, shares an educational background on one of the most common Moisture Associated Skin Damage (MASD) conditions: Incontinence Associated Dermatitis or IAD.
The inaugural Moisture Associated Skin Damage (MASD) Awareness Day, is a local and national driver to improve patient care and prevent skin damage as a result of moisture associated conditions. [1,2]
What is MASD?
MASD is a skin condition caused by overexposure of human skin to irritants such as urine, stool, perspiration, saliva, intestinal liquids from stomas and exudate from wounds.[3] Patient groups that are affected by MASD include those with complex health needs and reduced mobility, multiple comorbidities, or receiving cancer therapies.[4]
Exposure to irritants lead to compromised skin integrity and reduced barrier function, making the skin more permeable and susceptible to damage.[5] The global prevalence of MASD is not accurately reported, with great variability between clinical settings and geographical locations.[6,7,8] Patients affected by MASD can experience pain, burning and pruritus, discomfort and odour, which impact their quality of life.[5,6] Secondary infections can also develop, caused by fungi or bacteria, when the damaged skin is eroded.[4]
MASD covers an umbrella term including:
- Incontinence-associated dermatitis (IAD): Skin damage due to contact between the skin and urine and/or faeces.
- Intertriginous dermatitis: Skin damage due to sweat trapped in skin folds in areas with minimal air circulation .
- Peri-wound moisture-associated dermatitis: Skin maceration and breakdown caused by excessive wound exudate.
- Peristomal moisture-associated dermatitis: Skin damage due to interaction between the skin and stoma secretions.[3,9]
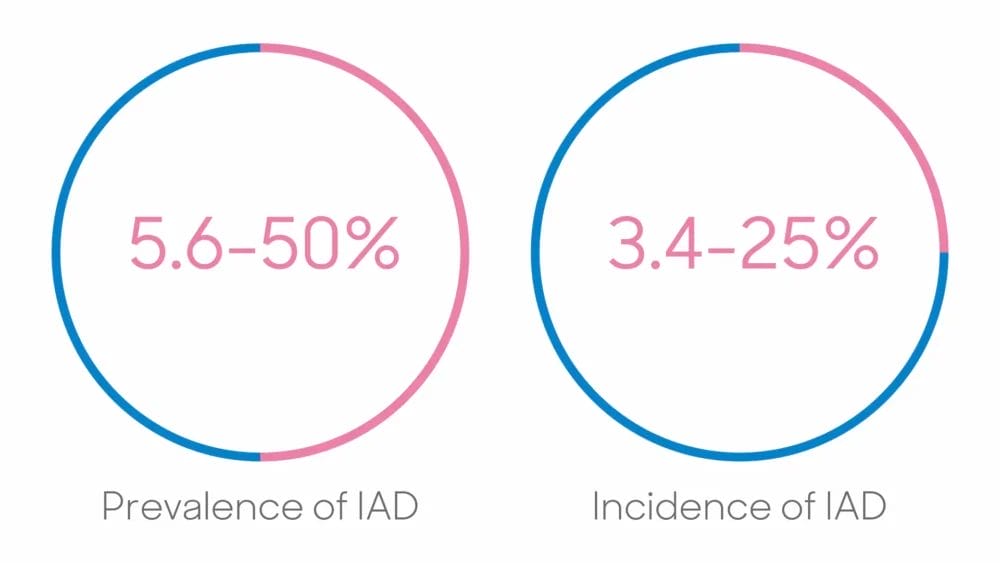
IAD is the most recognised form of MASD with variable incidence and prevalence rates due to a lack of consistent reporting, resulting in the Global IAD Expert Panel publishing best practice principles.[10]
What is IAD and how is diagnosed?
IAD is skin damage due to skin exposure to urine and/or stools. Parameters of IAD include: [3,10]
History: Urinary and /or faecal incontinence
Symptoms: Pain, burning, itching, tingling
Location: Perineum, perigenital, peristomal area, buttocks, gluteal fold, medial and posterior aspects of upper thighs, lower back
Shape/edges: Diffuse infected area with poorly defined edges/may be blotchy
Depth: Intact skin with erythema
Other: Secondary superficial infection might be present
Stages of IAD
The different stages of IAD include:[10]
Healthy

– No redness, intact skin
– No signs of IAD
Mild

– Red but skin intact
– Erythema, +/- oedema
Moderate-severe
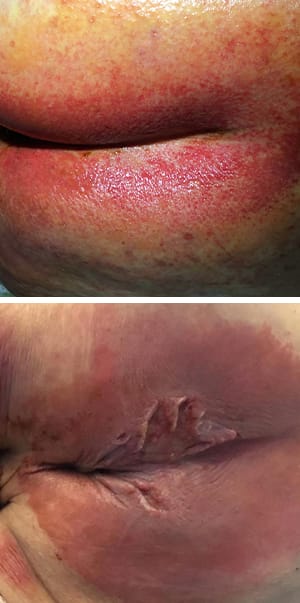
– Red with skin breakdown
– Erythema, +/- oedema
– +/-vesicles/bullae, skin erosion
– +/-denudation of skin
– +/-skin infection
Prevention of IAD
Evidence suggests a link between IAD and other skin conditions such as cutaneous infection and pressure ulcers.[11,12] According to IAD Expert panel, adopting a holistic, integrated approach, focused on prevention strategies and the importance of skin integrity is essential.[13] Early recognition of patients at risk is important, along with training and education of both caregivers and patients.[1,10]
Evidence from the Global IAD Expert Panel suggest two key interventions for the effective prevention of IAD:[10]
1. Manage incontinence
- Thorough assessment and cause identification to eliminate contact between skin and urine and/or faeces.
2. Structured skin care regime
- Cleanse the skin to remove urine and/or faeces.
Cleansers should be pH neutral. Non-rinse is preferred as prevents additional friction and addition of surfactant is preferred as it reduces surface tension and removes soil and debris from the skin with minimum force. Soap and water are not preferred as alkaline soap alters skin’s pH and damages skin barrier. Skin cleansers increase the likelihood of IAD healing by approximately 50%.[14]
- Protect the skin to avoid or minimise exposure to urine and/or faeces or friction.
Skin protectants form a barrier between the skin and the moisture or irritants such as urine and/or faeces. When IAD is present, protectants allow the skin barrier to recover and maintain hydration and trans-epidermal water loss.
- Restore skin’s integrity.
Is an additional step to support and maintain skin barrier function using leave-on products (moisturisers). They reduce dryness and aid overall health of the skin. Evidence showed that twice daily application of moisturiser, reduced the incidence of skin tears by 50%, in care home patients.[15]
Impregnated wipes in the prevention of IAD
A 3 in 1 pre-moistened wipe, incorporating cleansing, moisturising and protective functions has shown to be an effective intervention to prevent IAD in comparison to soap and water.[16,17]
Contiplan wipes has shown to offer 3 in 1 activity:[18]
- Cleanse: Cloths are wiped on the skin, which lifts and removes any dirt/external matter from the skin surface. Its chemical formula contains water and a range of surfactants that cleanse the skin.
- Protect: as it contains liquid paraffin (6%) and dimethicone (4%), which act as a protective barrier reducing moisture loss from the skin whilst also protecting it from external damage.
- Soothe: as Contiplan is rich in emollients, which make up 11.2% of the overall formulation.

Contiplan showed to offer positive barrier function by reducing transepidermal water loss (TEWL) and erythema.[18]
If you’d like more information, head to our Contiplan page. Help raise awareness about Moisture Associated Skin Damage (MASD) by sharing this article on social media.
[1.] Tyrer J. MINIMISE Moisture™: a local quality improvement initiative raising awareness of moisture-associated skin damage. Wounds UK 2021;17(1): 42-48
[2.] NHS Improvement. Pressure Ulcers: revised definition and measurement. https://www.england.nhs.uk/pressure-ulcers-revised-definition-and-measurement-framework/. Accessed March 11, 2022
[3.] Fletcher J, Beeckman D, Boyles A et al. International Best Practice Recommendations: Prevention and management of moisture-associated skin damage (MASD). London: Wounds International 2020. Available online at www.woundsinternational.com. Accessed on March 11, 2022
[4.] Gray M, Bliss DZ, McNichol L. Moisture-Associated Skin Damage: A Historic Step Forward. J Wound Ostomy Continence Nurs. 2021;48(6):581-583. doi:10.1097/WON.0000000000000827
[5.] Woo KY, Beeckman D, Chakravarthy D. Management of Moisture-Associated Skin Damage: A Scoping Review. Adv Skin Wound Care. 2017;30(11):494-501. doi:10.1097/01.ASW.0000525627.54569.da
[6.] Gray M, Black JM, Baharestani MM, et al. Moisture-associated skin damage: overview and pathophysiology. J Wound Ostomy Continence Nurs. 2011;38(3):233-241. doi:10.1097/WON.0b013e318215f798
[7.] Kottner J, Blume-Peytavi U, Lohrmann C. Associations between individual characteristics and incontinence-associated dermatitis: a secondary data analysis of a multi-centre prevalence study. Int J Nurs Stud. 2014;51(10):1373-1380. doi:10.1016/j.ijnurstu.2014.02.012
[8.] Beeckman D. A decade of research on Incontinence-Associated Dermatitis (IAD): Evidence, knowledge gaps and next steps. J Tissue Viability. 2017;26(1):47-56. doi:10.1016/j.jtv.2016.02.004
[9.] Yates, A. Incontinence-associated dermatitis 1: risk factors for skin damage. Nursing Times. https://www.nursingtimes.net/clinical-archive/tissue-viability/incontinence-associated-dermatitis-1-risk-factors-for-skin-damage-02-03-2020/ Published March 2, 2020. Accessed March 11, 2022.
[10.] Beeckman D, Campbell J, Campbell K, et al. Proceedings of the Global IAD Expert Panel. Incontinence associated dermatitis: moving prevention forward. https://www.woundsinternational.com/resources/details/incontinence-associated-dermatitis-moving-prevention-forward Published Febuary 13, 2015. Accessed on March 11, 2022
[11.] Jones JE, Robinson J, Barr W, Carlisle C. Impact of exudate and odour from chronic venous leg ulceration. Nurs Stand. 2008;22(45):. doi:10.7748/ns2008.07.22.45.53.c6592
[12.] Beeckman D, Van Lancker A, Van Hecke A, Verhaeghe S. A systematic review and meta-analysis of incontinence-associated dermatitis, incontinence, and moisture as risk factors for pressure ulcer development. Res Nurs Health. 2014;37(3):204-218. doi:10.1002/nur.21593
[13.] Beeckman D, Campbell K, Le Blanc K et al. Best practice recommendations for holistic strategies to promote and maintain skin integrity. https://www.woundsinternational.com/resources/details/best-practice-recommendations-holistic-strategies-promote-and-maintain-skin-integrity Published February 28, 2020. Accessed March 11, 2022
[14.] Glass GF Jr, Goh CCK, Cheong RQ. Effectiveness of skin cleanser and protectant regimen on incontinence-associated dermatitis outcomes in acute care patients: A cluster randomised trial. Int Wound J. 2021;18(6):862-873. doi:10.1111/iwj.13588
[15.] Carville K, Leslie G, Osseiran-Moisson R. The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. Int Wound J. 2014;11(4):446-453. Doi:10.1111/iwj.12326
[16.] Beeckman D, Verhaeghe S, Defloor T, Schoonhoven L, Vanderwee K. A 3-in-1 perineal care washcloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis: a randomized, controlled clinical trial. J Wound Ostomy Continence Nurs. 2011;38(6):627-634. doi: 10.1097/ WON.0b013e31822efe52
[17.] Beeckman D, Schoonhoven L, Verhaeghe S, Heyneman A, Defloor T. Prevention and treatment of incontinence-associated dermatitis: literature review. J Adv Nurs. 2009;65(6):1141-1154. doi:10.1111/j.1365-2648.2009.04986.x
[18.] GAMA Healthcare. Barrier protection study – 21.0226-44. proDERM Institut für Angewandte, Dermatologische Forschung GmbH, Schenefeld/Hamburg, Germany
SHARE THIS ARTICLE
Tags
Latest News
Celebrating 20 Years of GAMA Healthcare: Our Story
This month, GAMA Healthcare celebrates 20 years of helping prevent…
Norovirus: Understanding its transmission and prevention in the UK
Introduction Norovirus is recognised as the leading cause of viral gastroenteritis…
Clean Between to Reduce Healthcare-Associated Infections
Healthcare-associated infections (HAIs) are a significant concern for healthcare facilities…
Mpox: emergence of a new threat
A new threat related to mpox is emerging, in the…