Posted
21st August 2019
Research
Cleaning budgets are limited. Rational decisions must be made about purchasing cleaning and disinfectant products.
Evidence suggests disinfectant wipes save time and money when compared with other methods. In the landmark study by University Hospitals Birmingham (UHB), a time-consuming two-step process (involving the purchase of both a detergent and alcohol wipe) was replaced with a single-step cleaning/disinfection process using a Clinell Universal Wipe. Not only did the one-step process deliver operational benefits, the rate of MRSA was reduced by 55%.
One of the key advantages of one-step detergent/disinfectant wipes is their availability at the point of care. They also save nurses and cleaning staff time compared with other methods – such as conventional ‘mop and bucket’ type approaches.
Whilst one-step detergent/disinfectant wipes may appear, at face value, to be more expensive than other approaches, there are often multiple factors affecting cost-effectiveness. When evaluating any infection prevention strategy you should factor in the quality of the cleaning/disinfection process, any impact on Healthcare Associated Infections (HCAIs), staff time, and financial cost. For example, in one study, Clinell Sporicidal Wipes were found to offer the best balance between improved disinfecting performance and cost.
HCAIs can be very costly. Multiple published studies estimate HCAIs’ financial impact on healthcare organisations – and the financial benefit of achieving HCAIs reductions.
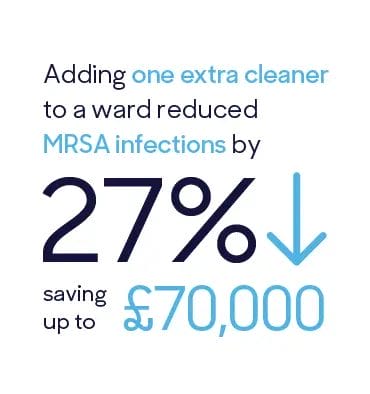
For example, a Scottish study found that providing an extra cleaner to a ward reduced MRSA infections by 27%. Because each MRSA infection was estimated to cost £9,000, this measure was actually calculated to save between £30,000 and £70,000 (saving provided as a range because of the inherent uncertainty in reduction achieved).
A similar calculation can be performed for the UHB study. In this study, introduction of Clinell Universal Wipes was associated with 55% reduction in rate of MRSA acquisition – falling from 20.7 to 9.4 per 100,000 patient bed days. We can determine that 64 MRSA acquisitions would be prevented each year (see Table 1 below).
A 2001 study found that the cost of MRSA colonisation was $1,363 which, when accounting for inflation, converts to £1,982 in April 2019. Therefore, the annual saving related to UHB’s reduced MRSA colonisation is estimated to be at least £126,848.
This figure is likely an underestimate: it only accounts for MRSA colonisation (asymptomatic), not MRSA infection. Some cases of MRSA colonisation would develop into infection, and infection is considerably more expensive than colonisation.
Also, whilst the study did not evaluate staff cleaning process time, it’s likely that the Clinell Universal Wipes one-step process was considerably quicker than the old two-step process, freeing up nurses to perform other tasks.
Table 1: Calculating the reduction in MRSA acquisitions
| – | Absolute value | Acquisition rate / 100,000 bed days |
|---|---|---|
| Bed days over 12 months | 565557 | – |
| MRSA acquisitions (measured) | 53 | 9.4 |
| MRSA acquisitions if no intervention (calculated) | 117 | 20.7 |
| MRSA acquisitions prevented | 64 | – |
SHARE THIS ARTICLE
Tags
Latest News
Celebrating 20 Years of GAMA Healthcare: Our Story
This month, GAMA Healthcare celebrates 20 years of helping prevent…
Norovirus: Understanding its transmission and prevention in the UK
Introduction Norovirus is recognised as the leading cause of viral gastroenteritis…
Clean Between to Reduce Healthcare-Associated Infections
Healthcare-associated infections (HAIs) are a significant concern for healthcare facilities…
Mpox: emergence of a new threat
A new threat related to mpox is emerging, in the…