Posted
3rd February 2023
Research
We originally wrote this post in 2015 as a briefing on various antibiotic resistant bacteria. It’s one of the most popular articles on the blog, so time for an update! Read on to discover more about “antibiotic-resistant Gram-negative bacteria” and why resistant Enterobacterales are a real cause for concern.
What are “antibiotic-resistant Gram-negative bacteria”?
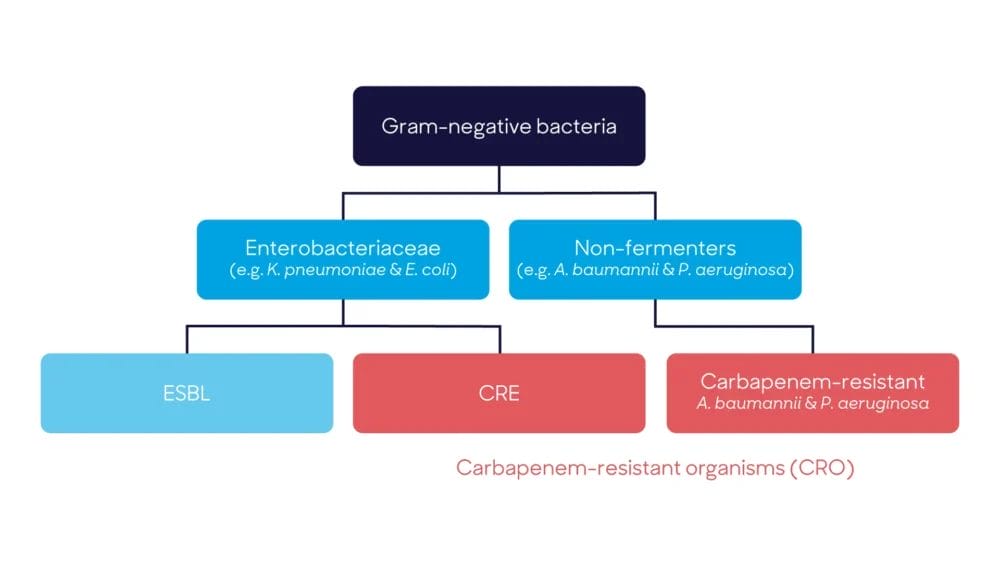
There is a group of bacteria known as “antibiotic-resistant Gram-negative bacteria” or “multi-drug resistant Gram-negative bacteria (MDR-GNB)”. This is a mixed group of various bacterial species and genera, with resistance to a variety of antibiotics. The flow-chart below illustrates the key groups.
Enterobacterales and non-fermenters
There are two families of Gram-negative bacteria that are resistant to key antibiotics: the Enterobacterales (previously known as Enterobacteriaceae) and non-fermenters.
The Enterobacterales (if you want to know how to pronounce ‘Enterobacterales’, this should help), including Klebsiella pneumoniae and E. coli, are the big concerns:
- Enterobacterales can be highly resistant to antibiotics.
- Enterobacterales are able to spread rapidly within a healthcare environment.
- Enterobacterales have the potential to establish a community reservoir.
- Enterobacterales invasive infections have a high mortality. A person with carbapenem resistance who is infected with Enterobacteriaceae has a 50% change of dying.
The non-fermenters include Acinetobacter and Pseudomonas. Although these bacteria typically have a high level of antibiotic resistance they are not that pathogenic and are rarely fatal. Therefore, the resistant Enterobacterales are the real concern.
Risk of CRE infections
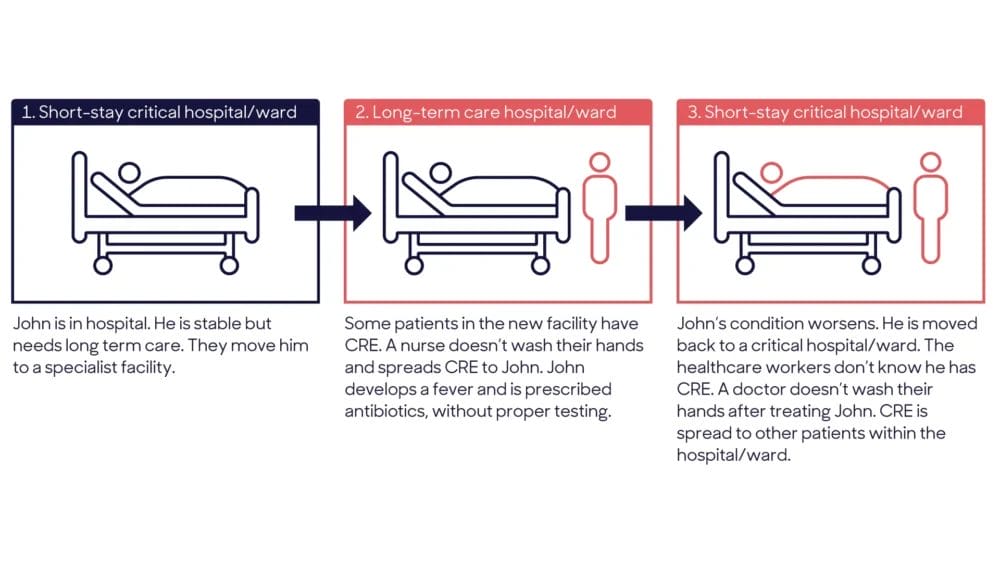
How CRE take over:
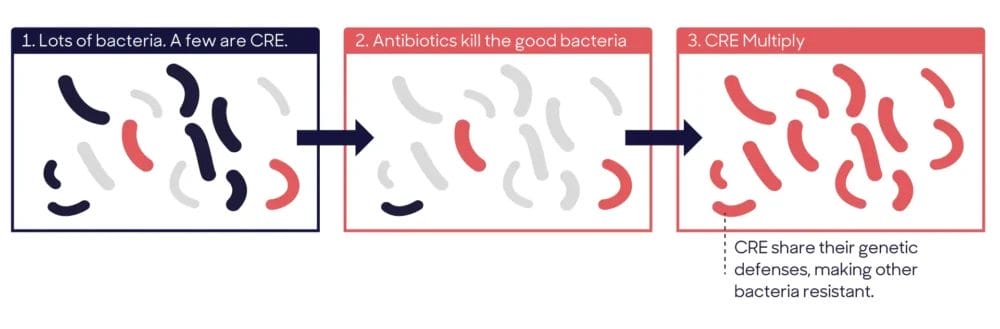
Resistant Enterobacterales
CRE and ESBLs:
Both carbapenemases and extended-spectrum beta-lactamases (ESBL) are enzymes produced by bacteria that can break down (“hydrolyse”) beta-lactam antibiotics. These enzymes occur within the Enterobacterales bacterial family, which includes E. coli and Klebsiella. They can cause infections such as urinary tract infections (UTIs), surgical site infections (SSIs) and blood stream infections (BSIs), and can also colonise the gut without causing symptoms.
What’s the difference between CREs and ESBLs?
Enterobacterales that are resistant to carbapenems by any mechanism are called carbapenem-resistant Enterobacterales (CRE) (those that produce carbapenemases are called ‘carbapenemase-producing Enterobacteriaceae’ (CP-CRE, or CPE for short)) and Enterobacteriaceae that produce ESBL enzymes are called ‘ESBLs’.
ESBLs produce an extended spectrum enzyme than breaks down and destroys most of the beta-lactams antibiotics such as penicillin and cephalosporins. But ESBLs have no effect on carbapenems (e.g., meropenem), the remaining beta-lactam antibiotic, so carbapenems are used to treat ESBLs. Now we are seeing the bacteria produce stronger beta-lactamases (carbapenemases) and these break down and destroy the remaining beta-lactam, carbapenem. So CREs are much stronger and more serious because few, if any, antibiotics are left to treat these. To make matters worse, the bacteria in this group can share the genes that make them resistant to antibiotics! Plus, the costs associated with the spread of carbapenem-resistant Enterobacterales in hospitals are significant.
Acronym guide for carbapenem resistance:
C: All the acronyms start with C
This is based on a type of very strong antibiotic called carbapenem. It is delivered intravenously and has always had a very effective broad spectrum of activity against all bacteria. Now we are starting to see Gram-negative bacteria becoming resistant to the carbapenem antibiotics which often means they are resistant to all other types of antibiotics. In the acronyms below, C refers to either the ‘carbapenem’ antibiotic itself, or the ‘carbapenemase’ enzyme that breaks it down.
P or R
P = producing and R = resistant
P is always twinned with carbapenemase (i.e. carbapenemase-producing) and R is always twinned with carbapenem (i.e. carbapenem-resistant). Put another way, you can’t have ‘carbapenemase-resistant’ or ‘carbapenem-producing.
O or E
O = organism and E = Enterobacterale
If you wish to refer to the Enterobacterales use ‘E’. If you wish to refer to a wider group of bacteria encompassing both the Enterobacterales and non-fermenters, use ‘O’.
Putting it all together:
Carbapenem-resistant organism (CRO)
These are all organisms (non-fermenters and Enterobacterales) resistant to carbapenems by a variety of ways – some by mutation, some inherent and some by producing a carbapenemase enzyme that breaks down the antibiotic.
Carbapenemase-producing organism (CPO)
These are all organisms (non-fermenters and Enterobacterales) resistant to carbapenems by producing carbapenemase enzymes that break down the antibiotic. CPO are a subset of CRO.
Carbapenem-resistant Enterobacteriaceae (CRE)
Enterobacterales that are resistant to carbapenems by a variety of ways – some by mutation, some inherent and some by producing a carbapenemase enzyme that breaks down the antibiotic.
Carbapenemase-producing CRE (CP-CRE, or CPE for short).
Enterobacterales that are resistant to carbapenems by producing carbapenemase enzymes that break down the antibiotic. CP-CRE are a subset of CRE.
We know this topic can be confusing, so if you have any questions, please get in touch on info@gamahealthcare.com. If you’d like to read more research from the GAMA Healthcare team head to the Research section on our blog. Help spread the word by sharing this article on social media.
SHARE THIS ARTICLE
Tags
Latest News
Introducing HEXI HUB: A seamless transition in our product line
We’re pleased to announce an update to our product offering…
Innovative solutions for tackling Carbapenemase-producing Enterobacteriaceae (CPE) at King’s College Hospitals
King’s College Hospital NHS Foundation Trust, one of London’s largest…
Gloves Off: reducing unnecessary plastic waste during environmental cleaning and disinfection
In this blog, Dr Phil Norville discusses the momentum-gaining ‘Gloves…
Gloves Off: Navigating SDS sheets and skin safety claims in environmental decontamination products
In this blog, James Clarke (Head of R&D, Science &…