Posted
19th December 2022
Products
In this blog post, we’ll uncover why Clostridioides difficile poses a challenge and how to best prevent the transmission of spores with commode decontamination.
Working in healthcare, “C. diff” is always a pathogen of concern. Rightly so, as it has been associated with costly outbreaks in healthcare settings, especially since the emergence of hypervirulent strains since the turn of the millennium.
With pharmaco-economists calculating the mean extra cost of a C. diff infection (CDI) at £10,965.82 per patient[1], the questions is: how can we keep total costs down?
Re-introducing C. diff
C. diff or, as it’s formally known, Clostridioides difficile (formerly Clostridium difficile) is a spore-forming bacterium that like many bacteria, lives harmlessly in 1 in 30 people’s gut flora[2].
However, CDIs are still prevalent. In Europe, each year there are:
- 152,905 CDI cases[3]
- 8,382 CDI-associated deaths[3]
What makes C. diff interesting is how infections occur… Antibiotics can actually disturb the balance of flora in the gut, resulting in the proliferation of C. diff and production of diarrhoea-causing toxins[4].
Spores, spread and susceptibility
Unfortunately, severe diarrhoea is a common symptom for patients with a CDI, and also provides millions of C. diff spores with a portal of exit. Contaminating surrounding areas, C. diff spores can spread via:
- Contaminated hands (of staff and patients)
- Contact with contaminated surfaces or equipment (including commodes)
Producing spores, tough bacterial structures, is one way bacteria can protect themselves from external threats. Coated in a thick spore coat, bacterial spores are less susceptible to disinfection and are therefore harder to kill, requiring higher level disinfection.
Related article: Why Clinell Peracetic Acid Wipes and other biocides are classed as sporicidal
Higher level disinfection
The term ‘higher level disinfection’ applies to the application of chemical biocides which are able to kill hard-to-kill pathogens, such as C. diff spores. Using appropriate disinfection methods is a sure way to reduce the number of spores in the environment.
Fully sporicidal (spore-killing) products can be challenging themselves, especially chlorine which calls for high and damaging concentrations to have the desired effect.
Peracetic acid is recognised as an effective sporicidal agent, and is the active biocide in Clinell Peracetic Acid Wipes – the first and only fully sporicidal wipe that is able to harness the power of peracetic acid in an easy-to-use format.
Related article: Peracetic Acid Wipes: A new name for Clinell’s red wipes
Easy-to-clean equipment
Shared patient equipment poses a significant infection risk, and commodes are no exception. In fact, because C. diff spread through faecal matter, bed pans, toilets and commodes are more likely to harbour spores unless thoroughly decontaminated.
Decontaminating commodes is critical but can be difficult and time-consuming, with intricate framework and crevices which can harbour hard-to-reach spores.
It’s important to invest in equipment that makes decontaminating easier for the user. Helping you get the best out of disinfection efforts, our Easyclean Commode can be dismantled and has no nuts, screws or bolts.

How to decontaminate a commode
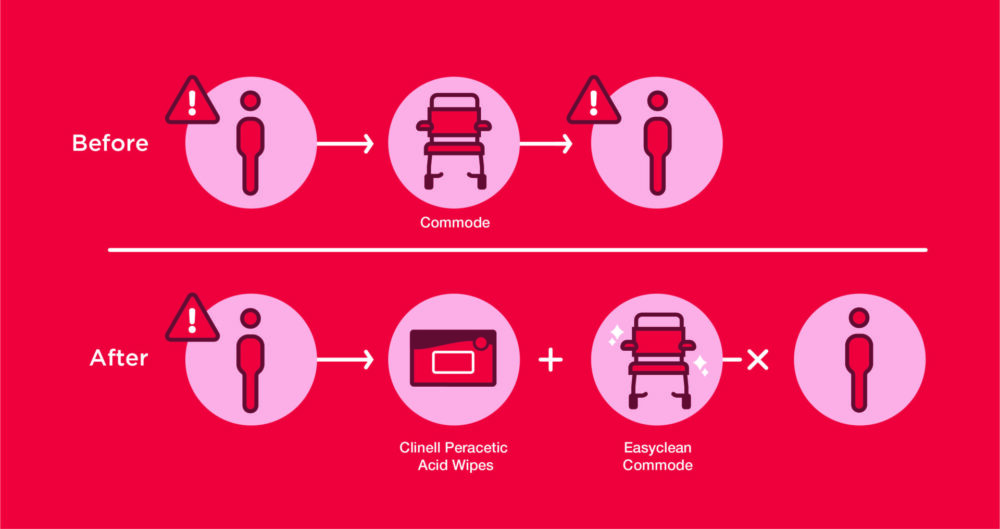
C. diff spores can survive in the environment for months or even years if equipment isn’t adequately decontaminated. Therefore, a combined approach using an Easyclean Commode and Clinell Peracetic Acid Wipes is recommended for the best results.
Download your free copy of the Clinell Cleaning Protocol.
The video below will take you through a step-by-step protocol for effectively decontaminating commodes.
For more information about solutions for managing C. diff in your hospital, please reach out to your local GAMA Healthcare Representative or contact us online.
References:
[1] Nakamura et al. Health-Economic Evaluation of Clostridium difficile Infection (CDI) And Epidemiology in England and Merseyside. Value Health. 2015;18(7):A582. DOI: https://doi.org/10.1016/j.jval.2015.09.1947
[2] NHS Inform. Clostridium difficile.https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/clostridium-difficile#:~:text=difficile-,C.,which%20can%20cause%20the%20C. Last updated Dec 6, 2022. Accessed Dec 16, 2022.
[3] Wiuff C et al. The Need for European Surveillance of CDI. Adv Exp Med Biol. 2018;1050:13-25. doi:10.1007/978-3-319-72799-8_2
[4] Community Infection Prevention and Control Harrogate and District NHS Foundation Trust. Community Infection Prevention and Control Policy for Care Home settings: Clostridioides difficile. Published Jul, 2020. Accessed Dec 15, 2022.
SHARE THIS ARTICLE
Tags
Latest News
Introducing HEXI HUB: A seamless transition in our product line
We’re pleased to announce an update to our product offering…
Innovative solutions for tackling Carbapenemase-producing Enterobacteriaceae (CPE) at King’s College Hospitals
King’s College Hospital NHS Foundation Trust, one of London’s largest…
Gloves Off: reducing unnecessary plastic waste during environmental cleaning and disinfection
In this blog, Dr Phil Norville discusses the momentum-gaining ‘Gloves…
Gloves Off: Navigating SDS sheets and skin safety claims in environmental decontamination products
In this blog, James Clarke (Head of R&D, Science &…